The 5 Ps of Successful Breastfeeding
Plan, Position, Practice, Patience and Persistence.
1. Plan and Decide if Breastfeeding is For You.
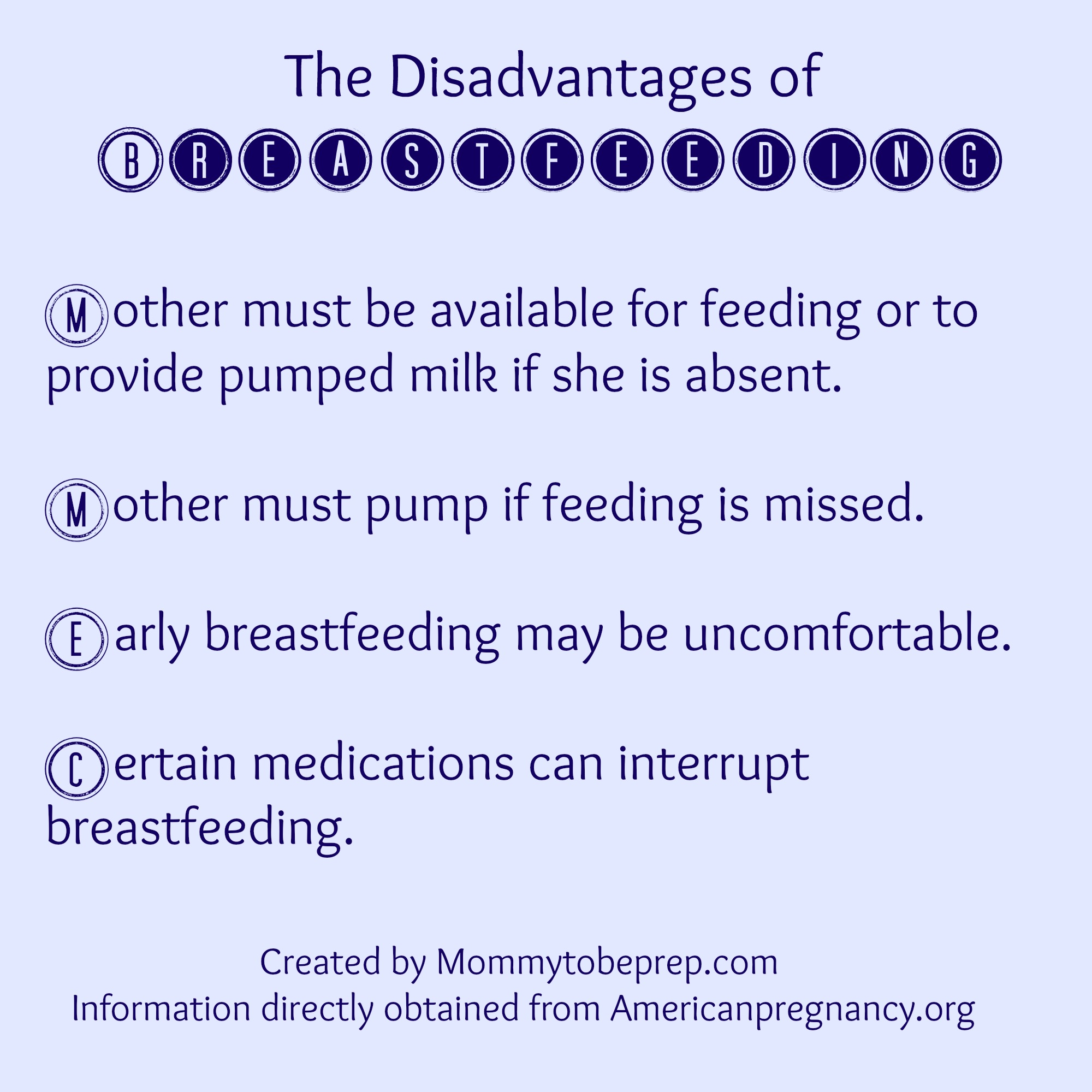
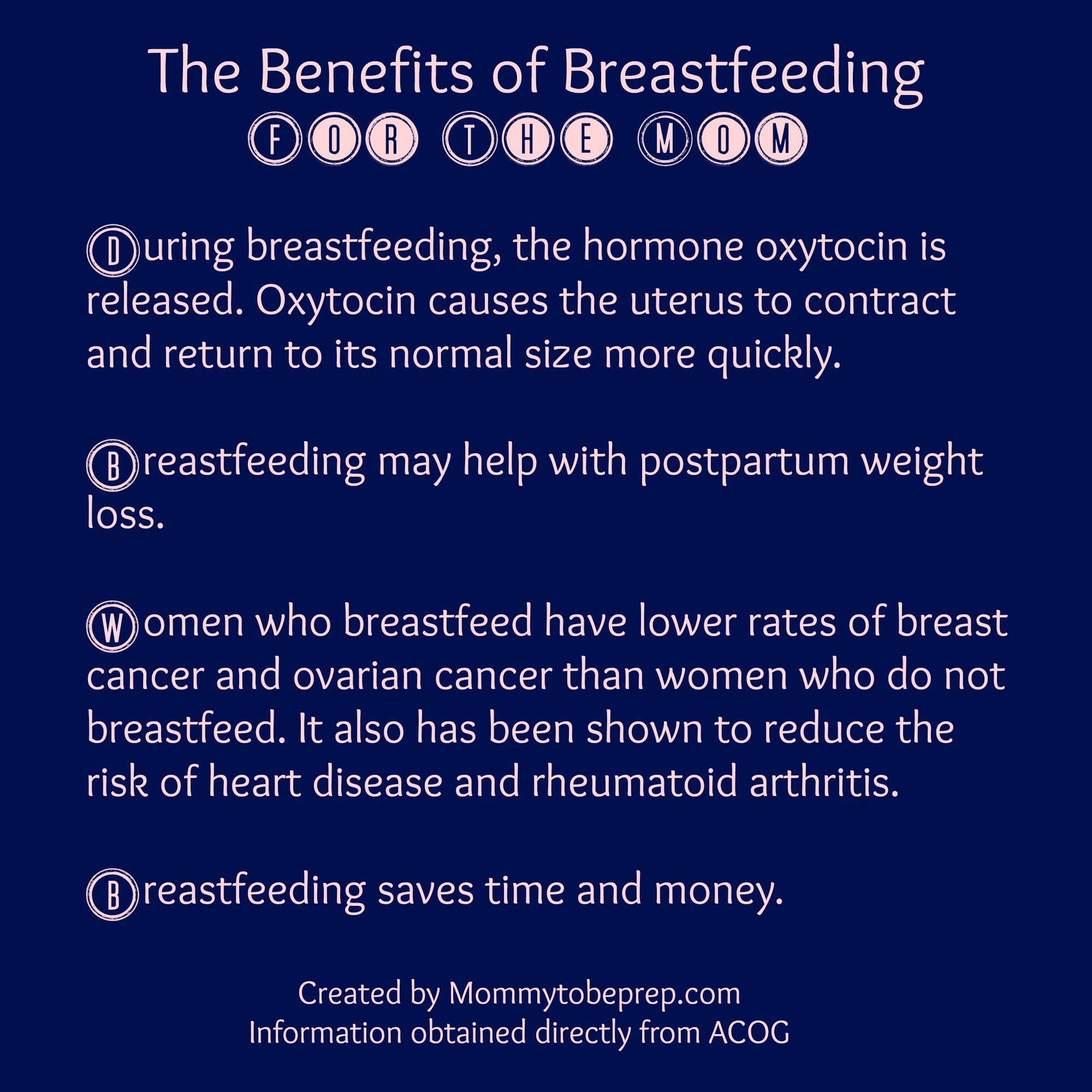
The pros and cons of breastfeeding should be understood when deciding if breastfeeding is for you and your baby. It is a good idea to discuss these with your health care team, but it is ultimately up to the parents to decide. Whether you have breasts the size of prunes, peaches, or pumpkins, the payoffs of breastfeeding are far reaching.

If you decided breastfeeding is for you, then H00RAY! Lets get planning and headed towards success!
– Sign up for a breastfeeding class held by a lactation consultant in your area.
Check with the hospital where you plan to deliver, as they may offer breastfeeding classes at no charge.
– Gather breastfeeding supplies.
- Invest in a nursing pillow/”Boppy Pillow” or put this on your birth registry.
- Add a nursing bra to your registry as well! Just teasing, you will probably need to be the one to find that perfect nursing bra for you! The fitting of the bra is very important as this can influence your milk supply.
- The hospital will usually be able to offer you some disposable breast pads to get you started, but you will need much more than that little free pack!
- A nursing cover that has a full 360-degree coverage and has a wide enough neck to take a peek at that beautiful babe! The one pictured above is my favorite and is from Covered Goods. Plus, it’s your lucky day! I am doing a GIVEAWAY on my Instagram for $25 shop credit to Covered Goods!- Check it out here: GIVEAWAY
- To prevent cracked nipples, the right latch is key, but also moisturizing Lanolin cream may work wonders. Your hospital or your provider usually will have a sample for you to try before you purchase a larger supply. I have also had patients use coconut oil as a nipple moisturizer.
- Soothie gel pads may also be a major relief for sore nipples. I would have a couple of these on hand for when you come home from the hospital. I like to pop these in the fridge an hour before giving them to my patients for extra relief.
- A breast pump is a necessity if you are planning on being away from your nursing baby for longer than three hours. Under the Affordable Care Act, “Health insurance plans must provide breastfeeding support, counseling, and equipment for the duration of breastfeeding. These services may be provided before and after birth. Your health insurance plan must cover the cost of a breast pump. It may be either a rental unit or a new one you’ll keep. Your plan may have guidelines on whether the covered pump is manual or electric, the length of the rental, and when you’ll receive it (before or after birth)” (Healthcare.gov).
Plan on doing skin-to-skin (kangaroo care) as soon as possible after delivery.
After delivery, we encourage you to do skin to skin with your baby if the circumstances allow. Skin-to-skin contact helps your body release hormones to make your breastmilk flow! Skin-to-skin will also help your baby see and smell your breasts and be encouraged to feed (UNICEF). The first hour after delivery, termed “the golden hour,” is when your baby is most alert. This is the best time to begin breastfeeding.
2. Positioning Yourself and Baby for Breastfeeding.
Position yourself.
- Make sure you are comfortable and in a place that you can relax.
- Support the baby in your arms with pillows.
- Prop your feet up to assist with relaxation and good posture.
- Always bring your baby close in to you, instead of you leaning forward to get to your baby. This prevents you from slouching forward, which may cause an inappropriate latch as well as stiffness and soreness in the mother’s shoulders and neck.
There are many terms for different positions out there for breastfeeding. The four main terms are; cross-cradle hold, cradle hold, football hold, and side lying. The important thing for you to know is this, use whatever position feels most comfortable for you and for your baby. In depth descriptions of these holds can be found at Americanpregnancy.org and pictures can be found all over google. The information for positioning your baby below, applies to all of these positions.
Position your baby.
- Bring your baby’s belly to your belly.
- Align your baby’s ear, shoulder, and hip so it makes a straight line. This makes swallowing for your infant much easier (try to look over your shoulder and swallow)… not easy right?
- Match your baby’s nose up to your nipple.
- Use one hand to hold your breast to help guide the nipple towards the baby’s top lip or nose. TIP: keep a broad grasp on your breast and do not grab the areola of the breast as this can cause the nipple to dimple inward.
- I like to compare holding the breast to the baby’s mouth to an adult taking a bite of a juicy hamburger. A hamburger best fits in your mouth horizontal, eating a hamburger vertical would just not fit and you would get less of the actual burger in your mouth! Hold your breast to the baby’s mouth like you are feeding them their first hamburger… (only the most nutritious and delicious hamburger they will every have!)
- Rub your nipple across your baby’s top lip and wait for him/her to open their mouth wide with their tongue down. TIP: make sure your baby’s chin is off their chest, as this can close off their airway.
- When your baby opens their mouth wide, bring them in close (close enough the baby’s chin should indent the lower part of your breast). TIP: It may take multiple attempts to get your baby to open their mouth wide. Do not force your nipple into the baby’s mouth, but instead rub the nipple again on the lips or chin of the baby and wait for their open mouth response.
- Try to get a silver dollar size chunk of the breast into your newborn’s mouth. TIP: If your baby has a shallow latch it will be more painful and the baby will get less milk. You will want to fit as much of your breast into your baby’s mouth for a deeper latch. Try running your own tongue on the roof of your mouth starting by your front teeth all the way back to where your teeth end. Do you feel the difference? The roof of your mouth turns from a hard palate to a soft palate. When breastfeeding, you want your breast to be able to reach all the way back to the baby’s soft palate for more comfortable breastfeeding experience and greater milk supply.
- Once your baby is latched, check to see if your baby’s lips are flanged out like fish lips! If not, use your finger to flare their lips for a better latch.
3. Practice Breastfeeding!
 Breastfeeding can be a difficult skill and needs to be practiced to be mastered. Babies are born with the natural instinct to breastfeed, but they too need the practice just like their parents! Notice I say parents and not just mother. Breastfeeding can be a joint practice. Many times in the beginning stages of breastfeeding, it takes four hands to keep the baby in the right position, latched, and alert for a full feeding! But don’t worry, it gets easier and easier with more practice!
Breastfeeding can be a difficult skill and needs to be practiced to be mastered. Babies are born with the natural instinct to breastfeed, but they too need the practice just like their parents! Notice I say parents and not just mother. Breastfeeding can be a joint practice. Many times in the beginning stages of breastfeeding, it takes four hands to keep the baby in the right position, latched, and alert for a full feeding! But don’t worry, it gets easier and easier with more practice!
4. Patience With Your Baby and Yourself While Learning and Mastering Breastfeeding.
When working with mothers on breastfeeding, I have noticed the babies sense and mimic their mother’s emotions! If the mom starts becoming frazzled or stressed that the baby is not latching appropriately, the baby will become frazzled too. When the mother is able to stay relaxed and calm, it helps to sooth the baby, and the two can work better as a team. Remember, you are both learning together.
5. Persistence in The Continuation of Breastfeeding.
Breastfeeding gets easier and easier with practice and the work does pay off, just stay with it!
How often and long should you breastfeed?
Each baby and mom are different. Womenshealth.gov recommends newborn babies breastfeed at least 8 to 12 times every 24 hours (every 2-3 hours) to help bring in your milk supply. Follow your baby’s schedule and adapt to them. Each feeding may be 15-20 minutes but there is no set time! Your baby will let you know when they are finished.
How do you know your baby is getting enough?
When you first begin to breastfeed, your baby’s stomach is very tiny! It starts off the size of a cherry and by three weeks it develops into the size of an egg. Although the baby’s stomach is small, it is a common fear for the mother that she is not producing enough milk for her baby.
You can be reassured you are producing enough milk for your baby by self expressing from the other nipple your baby is not breastfeeding from. This way, you can see approximately how much milk you are giving to your baby. You can also know your baby is getting enough milk when he or she shows signs of being more content and satisfied after feedings. The amount of wet diapers the baby has within a 24 hours lets us know if the they are hydrated. Your baby should have at least one wet diaper the first day, two wet diapers the second, three wet diapers the third and four wet diapers the fourth day (easy rule right?) Thank goodness the rule doesn’t continue much past that! By day five and after, your baby should have at least six wet diapers a day. Your baby’s weight will also be tracked daily while at the hospital. It is normal for newborns to lose up to seven percent of their birth weight within the first three days of delivery. Your pediatrician will inform you if your infant’s weight ever becomes concerning.
To see a visual chart of this information click here.
When should you stop breastfeeding?
Any amount of breastfeeding is better than none, but The American Academy of Pediatrics recommends babies be exclusively breastfed for “about the first six months of life. This means your baby needs no additional foods (except Vitamin D) or fluids unless medically indicated. Babies should continue to breastfeed for a year and for as long as is mutually desired by the mother and baby.” The World Health Organization (WHO) recommends babies to be breastfed even longer, “Exclusive breastfeeding is recommended up to six months of age, with continued breastfeeding along with appropriate complementary foods up to two years of age or beyond.”
Where can you find extra support and guidance for breastfeeding?
- You may call the National Breastfeeding help line at 800-994-9662 available Monday-Friday 9am-6pm EST. You will be connected to to a breastfeeding peer counselor that can help answer common breastfeeding questions and help you decide if you need more assistance from a doctor or lactation consultant.
- You may visit http://www.ilca.org to find an International Board Certified Lactation Consultant in your area.
- Find a local breastfeeding support group online through Facebook.
- Utilize The Women Infant and Children program (WIC) provided to low income families. For local WIC information visit http://www.fns.usda.gov/wic/breastfeeding/breastfeedingmainpage.htm or you may call the national office at 703-305-2746.
The woman body is “UDDERLY” amazing to support and give life to another growing human! You can do this. Just remember…
Plan, Position, Practice, Patience and Persistence.