13 Commonly Asked Questions Regarding C-Sections

Video created by my dear friend from West End Creative Group, see more of their beautiful videos at westendcreativegroup.com. Schedule with them and use the code westendbabies for a 10% discount!
My heart sympathizes when I see my laboring patient’s eyes swell with disappointment and fear when the Doctor breaks the news that they feel a C-section is in the patient’s best interest. Sometimes this information can be relayed in an emergent matter, quickly and proficiently as the mother is speedily rolled to the O.R. Sometimes it can be relayed in a softer manner that gives the family time to wrap their thoughts and emotions around the new idea of a C-section. Either way, this news can be scary and create a lot of emotion! But, as you can see in the video above of Lily’s birth, a C-section still brings a beautiful gift. My goal in writing this post as a L&D nurse is to help ease your fear by giving you the knowledge necessary to help you feel included and prepared for this possible emergent decision.
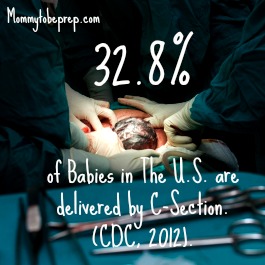
1: How Likely is it That I Will Need a C-Section?
The CDC reports that in 2012 33% of all births in the United States were completed via Cesarean section, this is the highest rate ever recorded in the United States! There are a few speculations as to why this percentage has reached such high numbers. These include an increase in multiple births (twins, triplets, etc.), older maternal age, more conservative practices, legal pressures, and the to-be-mother’s elective decision. There is a hope to see this percentage decrease as HealthyPeople.gov has set the goal to lower the rate of C-sections among low risk women by a whole ten percent. In my experience, most Doctors and Nurses really do not want to do a cesarean section for you, unless they really do believe it is safer for you and baby.
2. Why Would I Need a C-Section?
Most people do not plan on having a C-section, but as you’ve just learned, they may be more common than you had thought!
Multiple Pregnancy
Twins or triplets or more, puts you at higher risk for a cesarean delivery. The more babies inside your belly, the greater likelihood you qualify for a cesarean. This is because the babies may not be well aligned in the uterus, as well as the mother being more at risk for going into preterm labor. A C-section delivery may put less strain on the pre-term baby’s body. “Multiple pregnancy” accounts for an estimated 7% of C-section deliveries.
Failure of Labor to Progress
This is when the mother’s contractions do not adequately dilate the cervix to allow baby to pass through. A new study has shown that Doctors may need to be a little bit more patient until coming to this conclusion. See section “How long will it take me to dilate from 1cm to 10cm?” for more details. Failure of labor to progress accounts for an estimated 34% of C-section deliveries; this has been the most common reason for C-sections.
Fetal Intolerance
We Labor and Delivery nurses are always watching your little one’s heart rate pattern when you are on the monitor. You might even think we are obsessed over it, as we are documenting every 15-30 minutes, interpreting how your little one is doing. This helps us to see if your baby is getting enough oxygen and nutrients at all times. If there is an umbilical cord kink or pinch that does not get resolved with some positional changes and interventions, this may earn an emergency trip to the O.R. Fetal intolerance accounts for an estimated 23% of all C-section deliveries.
Placenta Problems
By observing your baby’s heart rate patterns, we can see how well the placenta is feeding your baby oxygen. “Placenta Insufficiency” is when the baby is not getting enough oxygen and nutrients from the placenta. Placenta insufficiency may be caused by smoking, high blood pressure, diabetes, or if the mother is significantly past her due date. Other major placenta problems include placenta previa (when the placenta blocks the passageway for baby to come out) and placenta abruption (when the placenta comes off of the uterine wall).
Big Baby
A large baby also called macrosomia, may be caused by gestational diabetes or being past due, but sometimes babies are just big! Your Provider may diagnose you with Cephalopelvic Dissproportion (CPD), meaning your baby’s head is too big, or your pelvis is just too small for baby to fit through. I heard a Doctor once liken CPD to a child’s block toy. The Doctor likened the baby’s head to a circle block and the mother’s pelvis like a square opening- not allowing the block to pass through.
Malpresentation
A malpresentation is when any any part of babe’s body is presenting other than a vertex presentation (the top of the head coming out first). A malpresentation is estimated to account for 17% of all C-sections.
Breech Presentation
According to Americanpregnancy.org breech babies occur approximately 1 out of 25 full term births, equaling 4% of babies (American Pregnancy Association, 2014).
Maternal Infection
Your temperature will be monitored during labor and especially close after your membranes rupture (amniotic fluid bag breaks). If your temperature increases to a fever, your Provider may call it quits on the vaginal route in order to be delivered as soon as possible to prevent further complications. Other infections such as Human Immunodeficiency Virus (HIV) or active Herpes will also warrant a C-section to protect the baby.
Maternal Condition
Most common conditions include preeclampsia, eclampsia, and gestational diabetes. In these situations, the Physician may decide it safer not to put the woman and baby under the stresses of labor.
* Information obtained from The American Congress of Obstetricians and Gynecologists May 2011 and March 2014.
Your OBGYN or Family Physician is the best person to help you make the decision if a cesarean delivery is most appropriate for you and your baby or babies.
3. Is There Anything I Can Do to Prevent a C-Section?
There are aspects that you have control over, such as, not smoking, eating healthy and following your Doctor’s instructions. These will help prevent an unwanted C-section; but, there are also aspects that you do not have control over. Try to let any fears regarding these uncontrollable circumstances go. Leeeetttt ittttt gooooooo, let it go! They do not serve you and actually may hinder your labor by creating fear and anxiety, so Relax! I understand this is easier said than done, but let me give you an incentive… A Norwegian study of 2,206 women with intentions on a vaginal delivery were assessed to determine their level of fear regarding giving birth. A significant level of fear was found in 7.5% of these women. These ladies, with an increase in fear, were found to have on average, a 47 minute longer labor and were also more likely to deliver by emergency C-section (10.9% of the women that were fearful, ended with a C-section, versus 6.8% ending in a C-section, without fear) (Adams & Eskid, 2012). That being said, don’t be fearful of being fearful… have a little faith and relax. 🙂
4. How Does a C-section Recovery Differ from a Vaginal Recovery?
A Cesarean section is a major surgery and is usually a longer and more extensive recovery than a vaginal delivery. A women with a C-section delivery usually stays in the hospital three days, versus a vaginal delivery of two days. The abdominal incision will be sore for the first couple of days and your physical activities will be limited. Upon returning home, plan to have someone stay with you to help you with your baby and other responsibilities you may have.
Tips to cope with the pain: For the first couple of days it’s a good idea to stay on top of your pain medications, see your options in The Most Common Medications in a Labor & Delivery Nurse’s Tool Kit. Tordol, Percocet, Ibuprofen, and Simethicone are some of the most common medications a delivered C-section patient will take to assist with the soreness (incisional), cramping (uterine cramps), and gas pains (often felt in the abdomen, neck, or right shoulder). Also, try to walk around the day after your surgery as much as you can as this keeps the blood flowing and prevents your lungs from getting lazy. Some physicians will recommend an “abdominal binder” this is kind of like a corset around your belly to help support the area. You can either purchase one before hand or the hospital may have one for you. Also, heating pads such as k-pads are a good idea to alleviate cramping and are offered by most hospitals.
Patients with cesarean sections are sometimes surprised to have vaginal bleeding for several days after delivery, this is actually normal. Another surprise may be that Doctors recommend nothing in your vagina (tampons, intercourse, douching) for about six weeks to allow the pelvic cavity to heal and return back to normal.
5. Can Someone Be In The O.R. With Me?

Most hospitals only allow one person to come in the O.R. with the patient. This special person will dress in a hair net, a facemask, a white body suite (we call it the bunny suite) or scrubs, and shoe covers. The person will be able to sit next to the patient’s head and will be able to stand up to see the baby born. That is… if they are okay with seeing blood and getting acquainted with the insides of their significant other.
6. Who Else Will Be In The O.R.?
The O.R. team for a cesarean delivery is pictured above. Although, the picture does not feature the Neonatologist, Circulating Nurse, or the Nursery Nurse. Depending on the hospital and your own circumstances, you may have more or less people that assist you in the O.R. This team of people is there to keep things running smoothly, but most importantly to keep you and baby safe.
7. What Type of Pain Control/Anesthesia is Used for C-Sections?
“You will be given either general anesthesia, an epidural block, or a spinal block” (The American Congress of Obstetricians and Gynecologists, May 2011).
If you have already been in labor and have had a good working epidural and then the “decision for an incision” is made, the Anesthesiologist/CRNA will be able to use the working epidural to numb the lower half of your body. This epidural block allows you to be awake for the delivery of your baby.
For most scheduled C-sections the Anesthesiologist/CRNA will do a spinal block. This is when he or she injects medication right into the spinal fluid through your back. This method allows you to be awake during the delivery as well.
If the Anesthesiologist/CRNA is unable to do either of these due to a lack of time, general anesthesia will be used. When general anesthesia is used, you will not be awake during the delivery of your baby. General anesthesia may also be planned if you have a deformity of the spine, are obese, or have an intolerance of having a spinal block or epidural administered. Many patients have said that the spinal block/epidural block was no worse than getting an IV.
It is important to know, you will not feel pain during the operation, but if you are awake, you may feel some tugging and pulling sensations.
8. How Long Does a C-Section Take?
The cesarean section on average takes about 45 minutes but the patient is usually in the O.R. for about 90 minutes due to the set up and clean up (Dimitrov, Stamenov, & Krusteva 1999). In my experience, many patients are surprised how quickly the Surgeon is able to delivery the baby versus the time it takes the Surgeon to stitch the patient back up.
9. Can I Still Do Skin-to-Skin (Kangaroo Care) in the O.R.?
Skin-to-skin or “Kangaroo care” is when a naked infant is placed on it’s mother’s bare chest. It is recommended a newborn has skin-to-skin contact as soon as possible if not immediately after a C-section. Skin-to-skin has shown to “Increase breastfeeding initiation, decrease time to the first breastfeed, reduce formula supplementation in hospital, increase bonding and maternal satisfaction, maintain the temperature of newborns and reduce newborn stress” (Stevens, Schmied, Burns, & Dahlen 2014).
If you would like to do skin-to-skin after the birth of your baby via C-section, let your circulating nurse know. He or she can relay this to the whole O.R. team to support this. Some barriers that might inhibit you from doing skin to skin in the O.R. is if you had general anesthesia for your C-section, or if you or your baby are unstable. If you had general anesthesia or if you are unstable, your significant other may do skin to skin with the baby. A study in 2007 shows Kangaroo Care by the father still greatly benefits the baby and increases bonding (Erlandsson, Dsilna, Fagerberg, & Christensson, 2007).

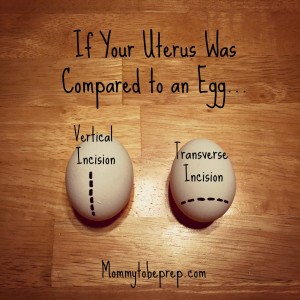
10. Where Will my Incision be?
There are two types of C-Section incisions, a vertical incision, which starts from the navel and extends to the pubic hairline and a transverse incision, which is horizontal across the pubic hairline (most bikinis will even hide the scar). Prior to a scheduled surgery, the nurse may use electric clippers to shave around where the incision will be. This doesn’t hurt, just may be a little ticklish! It is important to know that the “outside incision” through the skin and abdomen wall may be different than your “inside incision” on your uterus. A transverse uterine incision is the most common because there is less bleeding, heals well, and the chance for a vaginal birth for a future pregnancy is increased (John Hopkins Medicine).
The type of incision chosen will be your Physician’s choice and will depend on the mother and baby’s condition.
11. Is a Trial Of Labor After a Cesarean a Good Idea?
 Recently there has been a greater push towards a trial of labor after a cesarean delivery (TOLAC), and hopefully a successful TOLAC concluding with a vaginal birth after a cesarean (VBAC). A trial of labor is to assess how well the baby and mother do in in labor. In order for you to attempt a TOLAC, you will first need to weigh the risks and benefits with your OBGYN as each patient and circumstance is unique. Your OBGYN is best suited to help you with this decision as they know your medical history and have the knowledge and experience necessary. Your OBGYN will need to ensure there is no history of uterine rupture and will need to see the documentation of your previous cesarean delivery to ensure what type of incision you had on your uterus. Your Provider will also need to verify that she or he believes your pelvis is adequately large enough and that your baby is adequately small enough. Vertical incisions on the uterus should not attempt TOLAC due to the increase risk of uterine rupture. The hospital that you choose to do your TOLAC at must have the utilities and staff available to do a cesarean section in an emergency.
Recently there has been a greater push towards a trial of labor after a cesarean delivery (TOLAC), and hopefully a successful TOLAC concluding with a vaginal birth after a cesarean (VBAC). A trial of labor is to assess how well the baby and mother do in in labor. In order for you to attempt a TOLAC, you will first need to weigh the risks and benefits with your OBGYN as each patient and circumstance is unique. Your OBGYN is best suited to help you with this decision as they know your medical history and have the knowledge and experience necessary. Your OBGYN will need to ensure there is no history of uterine rupture and will need to see the documentation of your previous cesarean delivery to ensure what type of incision you had on your uterus. Your Provider will also need to verify that she or he believes your pelvis is adequately large enough and that your baby is adequately small enough. Vertical incisions on the uterus should not attempt TOLAC due to the increase risk of uterine rupture. The hospital that you choose to do your TOLAC at must have the utilities and staff available to do a cesarean section in an emergency.
Benefits
The benefits of a VBAC include no abdominal surgery, a shorter recovery period, a lower risk of infection, and less blood loss. VBACs can also help to prevent against bladder and bowel complications as well as placenta problems. This is because the more cesarean sections a patient receives, the more likely they will have these kinds of problems. Also, if you want to have many more kiddos a VBAC will help to prevent against a hysterectomy causing infertility (The American Congress of Obstetricians and Gynecologists August, 2011).
Risks
The risks of a TOLAC include possible rupture of the uterine scar or the uterus which can be seriously dangerous to the mom and baby.”TOLAC is associated with a perinatal mortality rate of 1.3 deaths per 1,000 births, compared with 0.5 per 1,000 births for elective repeat cesarean delivery” It is important to note that this rate is similar to that for all infants born to a first time mom (Leeman & King, January, 2011).
*A tip: Try to be as flexible as you can with your delivery plan, things can happen during pregnancy and labor that can make the risks or benefits outweigh one or the other. For example, if you are past your due date and you need to have your labor induced, your Doctor may want to revisit your decision on a TOLAC. Or, on the other hand, if you were planning on having a repeat C-section and your body goes into labor before your surgery, your Doctor may advise a TOLAC if you and baby are healthy as a C-section should only be done for a good reason.
12. How Long Should I Wait to Get Pregnant after a C-section?
Studies show that the chances of uterine rupture increase when the time between pregnancies after a C-section decrease. Women who had more than 18 months between their pregnancies had 86% chance of VBAC success. Women who had less than 18 months in between their pregnancies had a 79% VBAC success rate (Caughey, 2013). Consult with your OBGYN as well as your significant other to see when the best timing is for you.
13. How Many More Kids Can I have After My First C-section?
The answer to this question is very individual to the patient as many factors influence the answer. Again, your OBGYN will be best suited to help you with your planning. There is not a specific number of how many C-sections is safe for a mother but research does show that with each repeat C-section the chances for complications are increased. Dr. Roger Harms states, “Although there isn’t enough research to support a specific limit on repeat C-sections, most women can safely have up to three cesarean deliveries. Each repeat C-section is generally more complicated than the last” (Harms, 2012). If a mother is wanting to have a large family, she should make it her best efforts to have a vaginal birth after a cesarean (VBAC) to increase the chances of being able to carry and deliver more babies.
Story time!
During a C-section surgery, the surgeon is able to make an opening to visualize the pink shiny uterus either with retractors or with an instrument called an O-ring. I was the Circulator Nurse for this particular C-section when the Doctor paused to take notice and point out just how thin this mother’s uterine wall was. It was absolutely amazing to see, but also concerned us due to how thin the uterine wall had become. The usual thick pink uterus showed to be translucent. You could see parts of the baby’s body moving in the uterus! The Doctor stated to the patient they would need to re-discuss about having any more babies in the future.
Did you have an unplanned C-section and have any words of wisdom? If so, share bellow!
References:
Adams S, Eberhard-Gran M, Eskild A. Fear of childbirth and duration of labour: a study of 2206 women with intended vaginal delivery. BJOG 2012;119:1238–1246.
American Pregnancy Association (May, 2014). Breech Births. Labor and Birth. Retrieved from: http://americanpregnancy.org/labor-and-birth/breech-presentation/
Caughey, A. B. (August, 2013). Vaginal Birth After Cesarean Delivery. Medscape. Retrieved from: http://emedicine.medscape.com/article/272187-overview#showall
Dimitrov A, Stamenov G, Krusteva K. The Overall and Step-By-Step Duration Of Cesarean Section. Akush Ginekol (Soffia). 1999. Bulgarian. PubMed. PMID: 10734668
Erlandsson, K., Dsilna, A., Fagerberg, I. and Christensson, K. (2007), Skin-to-Skin Care with the Father after Cesarean Birth and Its Effect on Newborn Crying and Prefeeding Behavior. Birth, 34: 105–114. doi: 10.1111/j.1523-536X.2007.00162.x
Harms, R. W. (June, 2012). How Many C-Sections can a woman safely have? C-Section Retrieved from: http://www.mayoclinic.org/tests-procedures/c-section/expert-answers/c-sections/faq-20058380
HealthyPeople.gov. Maternal, Infant, and Child Health. 2020 Topics. Retrieved from: https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives
John Hopkins Medicine. Cesarean Delivery. Retrieved from: http://www.hopkinsmedicine.org/healthlibrary/test_procedures/gynecology/cesarean_delivery_92,p07768/
Leeman, L. M., & King, V. J. (January, 2011). Increasing patient access to VBAC: New NIH and ACOG recommendations. Retrieved from: http://www.aafp.org/afp/2011/0115/p121.html#afp20110115p121-b2
Menacker, F., & Hamilton, B. E. (March 2010). Recent Trends in Cesarean Delivery in the United States. NCHS Data Brief, number 35. Retrieved from: http://www.cdc.gov/nchs/data/databriefs/db35.htm#cesarean_by_state
Stevens, J., Schmied, V., Burns, E. and Dahlen, H. (2014), Immediate or early skin-to-skin contact after a Caesarean section: a review of the literature. Maternal & Child Nutrition, 10: 456–473. doi: 10.1111/mcn.12128
The American Congress of Obstetricians and Gynecologists (March, 2014). Safe Prevention of the Primary Cesarean Delivery. Obstetric Care Consensus Series. Retrieved from: http://www.acog.org/Resources-And-Publications/Obstetric-Care-Consensus-Series/Safe-Prevention-of-the-Primary-Cesarean-Delivery#79
The American Congress of Obstetricians and Gynecologists (May, 2011). Cesarean Birth (C-Section). Frequently asked questions labor, delivery, and postpartum care. Retrieved from http://www.acog.org/Patients/FAQs/Cesarean-Birth-C-Section#what
The American Congress of Obstetricians and Gynecologists (August, 2011). Patient FAQ: Vaginal Birth After Cesarean Delivery—Deciding on a Trial of Labor After Cesarean Delivery. Retrieved from: http://www.acog.org/Patients/FAQs/Vaginal-Birth-After-Cesarean-Delivery-Deciding-on-a-Trial-of-Labor-After-Cesarean-Delivery
Photo Credits:
Image courtesy of Arztsamui at FreeDigitalPhotos.net (13 Commonly Asked Questions Regarding C-Sections & How Likely is it That I Will Need a C-Section?)
Image courtesy of Patpitchaya at FreeDigitalPhotos.net (What type of pain control/anesthesia is used for C-sections?)
Image courtesy of Stock Images at FreeDigitalPhotos.net (How long does a C-section take?)
Image courtesy of Patrisyu at FreeDigitalPhotos.net (Is a Trial Of Labor After A Cesarean A Good Idea?)